Last updated November 2025
Providers forced to jump through hoops to get prior authorizations for patients know the pain of waiting. But, according to AHIP, prior authorizations ensure a patient gets safe, timely, evidence-based care that’s both affordable and efficient. To help providers ensure patients get that, try the tips in this prior authorization cheat sheet.
Health insurance companies have the unique advantage to see how a patient is utilizing their coverage and what treatments they have already received. The prior authorization process helps prevent duplicate and unnecessary tests and treatments while ensuring the patient is receiving the proper care for their condition.
How Do You Speed Up the Prior Authorization Process?
If, as a provider, you or your staff struggle with managing prior authorizations, try these steps to speed the help process up and prevent denials.
Cheat Sheet of Tips to Speed Up the Prior Authorization Process
- Have a master list of procedures that require authorizations
- Document denial reasons so you can avoid them in the future
- Sign up for payer newsletters to track prior authorization best practices
- Stay informed of changing industry standards, including prior authorization Medicare changes in 2026
- Designate prior authorization responsibilities to the same staff member(s) each time
- Inform your scheduling staff about procedures that require prior authorizations, so they can alert you — and your patients — early
- Keep information about authorization in a central location
- Use technology
- Create a quick reference guide of your payer contacts if you don’t have access to them in your EHR
- Thoroughly and regularly document clinical data
- Record all correspondence you have with a payer
- Create a follow up plan with your staff
- Be methodical about working prior authorizations
- Ask payers for an estimated turnaround time for an authorization
- Educate your patients on the prior authorization process
- Keep patients informed
Most Common Prior Authorization Challenges
In a poll taken during a past Azalea Health Prior Authorizations Best Practices webinar, 35% of respondents noted that “Delay of Care” is their top challenge with prior authorizations.
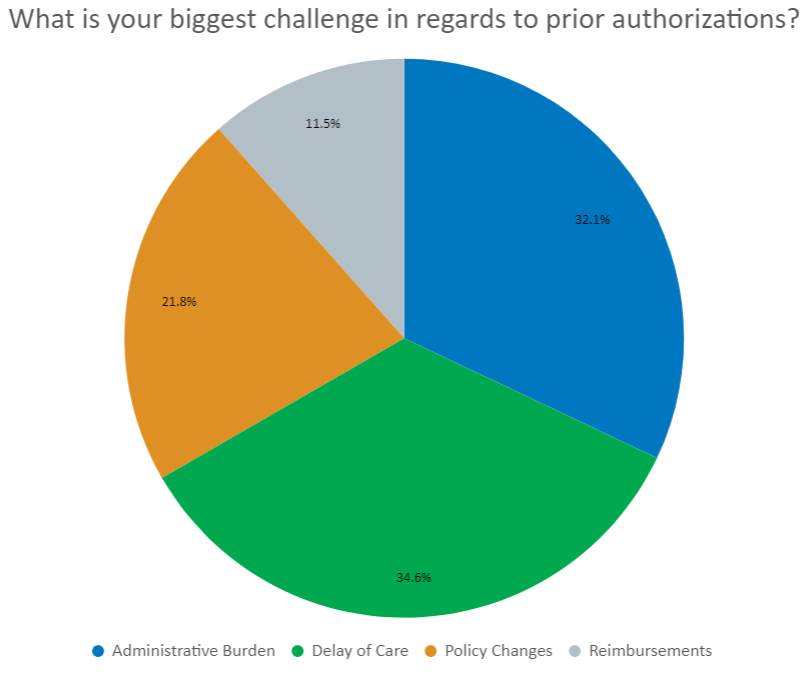
While another 32% selected “Administrative Burden” as their biggest challenge.
The following 16 tips from the prior authorization cheat sheet can help in both areas. Tips fall into five categories for managing prior authorizations in medical billing:
Cheat Sheet Tips 1–4 — Payer Requirement Prior Authorization Tips
One of the best tips for speeding up the PA process is to familiarize yourself with payer requirements. Every payer has their own. Different types of services have different requirements too.
Here are four tips to help you manage the requirements of each of your major payers.
1. Create a Master List of Procedures That Require Authorizations
When it comes to common procedures in your facility, create a list of procedures that require prior authorizations for each payer — and each payer’s plan potentially. This lets you streamline your process and reduce frustration, call times, and denials.
Tip! If you use the Azalea Hospital or Ambulatory EHR, Azalea Analytics lets you pull your payer mix and payer plan mix so you can easily identify the payers you need to track.
2. Document Denial Reasons
Anytime a prior authorization is denied, keep track of the reason, the payer, and the payer’s plan. Work on this document with the entire team to help prevent denials in the future.
Tip! If you use the Azalea Hospital EHR or Ambulatory EHR, Azalea Analytics lets you easily track denials and denials reasons. You get quick access to a comprehensive look back at denial information and an easy way to track reductions in the number of denials over time.
3. Subscribe to Payer Newsletters
Subscribing to payers’ newsletters lets you stay informed about updates, policy changes, and billing information that relates to their different approaches to prior authorizations.
4. Stay Informed of Changing Industry Standards
Take advantage of resources that let you keep track of industry requirements around prior authorizations. The American Medical Association and Centers for Medicare & Medicaid Services (CMS) offer the most up-to-date information.
Tip! CMS is mandating that prior authorizations for Medicare patients get turned around faster starting January 1, 2026. They’re also mandating the payers share denial reasons. Learn more about these mandates in Medicare changes in 2026 along with more changes coming in 2027 that will affect you and all payers.
Prior Authorization Cheat Sheet Tips 5–8 — Workflow Optimization and Efficiency
Providers and staff can spend more than 20 hours a week working on prior authorizations. That’s a lot of time that could be spent doing other things.
But, if you optimize your workflows to be more efficient, you can help reduce delays in patient care. Start with these four tips.
5. Designate Prior Authorization Responsibilities to the Same Staff Member(s) Each Time
Handling prior authorizations regularly makes staff more efficient and more aware of each payer’s requirements. Knowing what works and what doesn’t is key to speeding up the time it takes to get a prior authorization approved.
6. Tell Scheduling Staff About Procedures That Require Prior Authorizations
When the front office staff knows which procedures require prior authorizations in advance, they can make sure the patient gets scheduled for followups on a timeline that matches.
7. Keep Authorizations in a Central Location
If you use the Azalea Hospital EHR or Ambulatory EHR or something similar, you get the ability to track the authorization process. If your EHR doesn’t let you do that, consider adopting shared spreadsheets to help keep everything in one place.
8. Use Technology
Take advantage of the online payer portals for prior authorizations. The time it takes to initiate an authorization online is more than 50% faster than doing it by phone or fax.
And to really embrace technology, consider a tool like AI Billing Assistant. It will automatically flag claims that contain potentially avoidable denials.
Cheat Sheet Tips 9–11 — Prior Authorization Documentation
Documentation is a critical part of the prior authorization process, both for keeping your work list up to date and the processing of the authorization. Here are some best practices to document the prior authorization process.
9. Create a Quick Reference Guide of Your Payer Contacts
You know which payers you work with the most. Maintaining a list of ways to contact them will help you process prior authorizations more quickly.
10. Thoroughly and Regularly Document Clinical Data
One of the common causes for a denied prior authorization is a lack of clinical documentation. Ensure that your providers are accurately documenting in the patient’s chart, including ensuring their medications are up to date.
Tip! Consider ambient charting with a tool like AI Clinical Assistant, powered by Suki. It uses AI to augment and automate the charting process. It helps providers keep more accurate charts with less manual input and give them more patient face time.
11. Record All Correspondence You Have with a Payer
Keeping a record of who you spoke with, date and time, and a reference number will help if and when you need to appeal a denial.
Tip! If you’re sending supporting clinical documentation by secure fax, use a cover sheet that includes the pending authorization number(s) and your contact information.
Prior Authorization Cheat Sheet Tips 12–14 — Following Up on PAs
Even though most payers send notifications when an authorization’s approved, sometimes they don’t send them in real-time. For you, proactively following up on prior authorizations can help prevent delays.
12. Create a Follow Up Plan with Your Staff
Don’t rely on the payer to communicate approved authorizations in a timely manner. Follow up with them every 48 to 72 hours to ensure you’re informed of the status.
13. Be Methodical About Working Prior Authorizations
Prioritize the authorizations you need to work on by schedule date. And if you want to be even more efficient, group by payer to reduce the amount of time you spend shifting from payer to payer.
14. Ask for an Estimated Turnaround Time for the Completion of an Authorization
By having an estimated timeline, you can prioritize your follow ups per that timeline and put your time where it’s most needed.
Cheat Sheet Tips 15 and 16 — Patient Engagement
Patients are engaged in their care. And that means they want to know what’s going on, including some of the back office processes. When you take the time to inform your patients of the process, they’re more likely to tolerate delays in care.
15. Educate Patients About the Prior Authorization Process
Many patients aren’t aware of the complexities and time it takes to get an authorization from the payer. Educate them on the process to help set expectations and reduce potential frustration.
Even though more than 80% of PAs are approved, the other 20% are denied. Make sure your patients understand the possibility of denial and that they have the right to appeal. To set expectations, talk to them about the appeals process in the early stages. Also, make sure they understand that even if the PA is denied, you can help them appeal two or more times.
16. Keep Patients Informed
Keep your patients in the loop on the prior authorization process and the impacts it may have on getting their procedure scheduled. Patients are more likely to be patient if they know why they’re waiting.
Get Expert Help with Billing
If you’re after expert revenue cycle management help for your clinic or specialty practice, contact Azalea. Azalea RCM services can help you get paid faster.




